A professional’s guide to paediatric spinal injury
by Christine Batty
Introduction
Spinal Injury in children is quite rare, but can occur following traumatic birth, road traffic accident, falls, sports injuries or violence (such as stab wounds).
The spinal cord is a bundle of nerves, protected by the bony vertebrae of the spine that carries the messages from the brain to all parts of the body and back again.
Acute spinal cord injury (SCI) can result in bruising to the spinal cord (contusion), a partial or a complete tear or transection. This can cause permanent disability and even death.
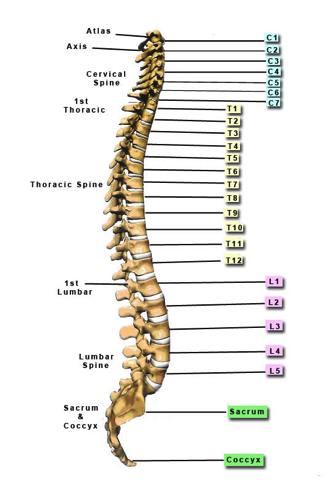
The severity of the injury depends on the part of the spine that is damaged. Neck (cervical spine) injuries can cause loss of movement and sensation affecting all four limbs, called tetraplegia. Damage to the spine just below the skull can cause death or inability to breathe unassisted, so that a ventilator is required to provide mechanical breathing as the muscles required for breathing may be paralysed.
An injury to the lower spinal cord (thoracic or lumbar region) can result in paralysis of the muscles and, loss of sensation in the legs, called paraplegia.
If the transection of the spinal cord is incomplete there may be partial paralysis or some sensation remaining below the level of the injury.
As well as paralysis and loss of sensation there may also be loss of bladder and bowel function, abnormal blood pressure control, sweating, shivering and involuntary muscle spasms.
Acute Stage
If emergency services attend at the time of the injury, the child will be fitted with a neck or spinal brace at the scene, which will remain in place until the doctors at A&E have assessed the likely damage.
Immediately following trauma to the spinal cord, there may be a period of spinal shock caused by bruising and swelling, which causes loss of movement, reflexes and sensation. As swelling subsides the symptoms that remain or develop give an indication of the extent of the damage that may be permanent.
There may be an initial period of bed rest to allow the bony spine to heal or the child may require surgery to stabilise the vertebrae. During a period of bed rest, nursing staff will attend to the child’s personal care and will turn them regularly to prevent the development of skin problems or pressure sores.
Treatment of spinal injuries usually takes place in a specialist spinal injury centre, some units having a separate children’s unit, where staff specialise in the treatment and rehabilitation of children with this type of injury.
Ventilated Children
Children that require ventilation may be cared for in paediatric intensive care, in the initial stages, and may require long term intervention from specialist teams. NHS England have developed a pathway for the care of children who require long term ventilation and further information can be found here:
These children will require high levels of care and parents and families will need hospital staff to liaise closely with community teams to make sure adequate care and support are available following discharge home.
Occupational Therapy
Kids Health Organisation gives the following very useful definition of the specialism of paediatric occupational therapy:
“Occupational therapy (OT) treatment focuses on helping people with a physical, sensory, or cognitive disability be as independent as possible in all areas of their lives. OT can help kids with various needs improve their cognitive, physical, sensory, and motor skills and enhance their self-esteem and sense of accomplishment. Some people may think that occupational therapy is only for adults; kids, after all, do not have occupations. But a child's main job is playing and learning, and occupational therapists can evaluate kids' skills for playing, school performance, and daily activities and compare them with what is developmentally appropriate for that age group.”
http://kidshealth.org/parent/system/ill/occupational_therapy.html
Rehabilitation and the role of the in-patient Occupational Therapist
Rehabilitation is most effective when a team of professionals (Multi-disciplinary team or MDT) work together, sharing information and providing a coordinated approach to treatment and discharge planning.
As soon as medical staff decide that the fracture or injury is stable, rehabilitation will begin.
At this stage the doctors should be able to discuss with the parents and child what they can expect in terms of recovery and what permanent disability may remain as a result of the injury.
Rehabilitation will aim to promote the maximum function and independence that the child can achieve.
The physiotherapist, occupational therapist and nursing staff will work as a team in treating the child and their roles often overlap.
The physiotherapist will prescribe exercises and may begin to get the child into a sitting position and work on balance in preparation for sitting out in a wheelchair or progressing to standing.
The occupational therapist will start to teach the child how to transfer out of bed using equipment such as a sliding board, if necessary, and into a wheelchair. The wheelchair may be self-propelled or some will require power chairs depending on remaining function.
Some children with cervical injuries may need to be hoisted to transfer out of bed, but with the correct controls or switches, may be able to use power wheelchairs.
The OT will work with the child to promote independent washing, dressing etc.
There will often be a teacher attached to the unit, who will see the child so that their education can continue as soon as possible once their condition stabilises.
Within the spinal injuries unit, children will always be encouraged to gradually take responsibility for their own independence and to do as much as possible for themselves, within the daily routine.
The physiotherapist may introduce some children (paraplegics and some tetraplegics) to various sports that can be done by wheelchair users. This can greatly enhance a child’s self-esteem and sense of being able to achieve something at this stage.
Some families and children may have trouble adjusting to the remaining disability and a psychologist, OT, may be able to help with this aspect of rehabilitation. Siblings of children with spinal injuries should be encouraged to visit and may also need help to adjust and to understand what has happened.
Discharge planning will start early on and the child and their family will be involved in this process from the outset. The OT will carry out a home visit, often with the Local Authority OTs from the child’s area, so that adaptations to the home can be planned or equipment can be ordered, so that everything is in place ready for discharge home. Children may be able to go home for short periods or weekend leave so that they can begin to understand what living back at home will be like and if there are any problems arise they can be dealt with before final discharge. Following a visit home, the OT will discuss with the parents and carers how this went and together will plan further visits or discharge.
Most spinal injury units keep children on their outpatient list long term so that they are a point of contact for any queries, ongoing treatment or advice.
Hospital doctors and therapists will pass on information to community services and will liaise with schools prior to discharge so that the transition to living back at home is as easy for the child and family as possible.
The role of an independent occupational therapist
An independent OT can be part of the MDT at any stage of the rehabilitation journey. If the case manager or family identify that they will be using an independent OT after discharge then it can be beneficial to appoint them prior, this allows them to liaise with their OT and other MDT colleagues to ensure a seamless hand over on the appropriate areas but also a collaborative approach on areas of therapeutic cross over.
Areas that that a paediatric OT will be able to support within the field of spinal injury include:
- Seating – static and dynamic
- Wheelchair accessible vehicle selection for family use.
- Moving and handling including hoists, slings, bathing, toileting, car hoists / transfers, internal and external home lifts.
- Housing – selection of temporary and permanent properties with a view to feasibility of adaptations. Specifications for home adaptations, equipment trial and recommendations, review of adaptation plans.
- Bathing – assessment and trial of bathing solutions, bathroom adaptations and equipment.
- Carer and family training
- Assistive technology – depending on the area of the spinal damage, assistive technology can play a large role in facilitating a child to be and grow to be as independent within their environment as possible. Ranging from simple hand held apps on mobiles or tablets to eye gaze systems for very high-level injuries.
- Access to education and hobbies.
- Teaching new techniques for example if a child experiences an injury in their infancy they will need to learn how to dress themselves as they get older and require more independence. Equally they may experience a spinal injury in early teens and the role of the OT maybe around facilitating independence with personal care.
The role of an OT is to look holistically at the child and their goals for daily life. Whilst this will initially focus around the home (sometimes multiple homes if respite care or separated parent families) it is also likely to extend across nursery, school, college and even university settings.
At all times the OT assessment and intervention focuses not only on the child with a spinal injury but also the family including other siblings to ensure that alternations, equipment or vehicles are as inclusive for every day family life as possible.
An OT, much like all professionals involved often has a long journey with the child and their family, once the OT has implemented adaptations, equipment and training they will then be required for regular reviews as the child grows, their needs change and the family dynamics alter – the birth of a new sibling or a change in parenting for example.
Useful Links
http://www.backuptrust.org.uk/what-we-do/children-and-young-people
https://www.rnoh.nhs.uk/clinical-services/spinal-cord-injury-centre/services-for-children
http://www.cafamily.org.uk/medical-information/conditions/s/spinal-injuries/
http://www.rcem.ac.uk/CEM/document?id=7931

